How your bladder works
Elaine Miller – part 2
If your bladder contracts with little or no warning, it can give you an urgent need to pass urine. This gives you little or no time to get to the toilet.
Uncontrolled bladder contractions are not dangerous but are a common cause of frequent voiding, a feeling of urgency and leakage of urine.
Your bladder’s job is to store urine. When it is nearly full, it sends a message to your brain that you “need to go”. Once you have found somewhere appropriate to urinate your bladder squeezes itself to completely empty – and then the cycle starts again.
Simple, right? We want people to understand how their bladder works, things which might help and where to seek help because if your bladder isn’t doing what you need it to do it, we know it impacts on your wellbeing.
People who are not confident that their bladder will work efficiently are more likely to: be anxious or depressed; less likely to be physically active; more likely to need time off work and less likely to have satisfying intimate relationships. We know that the worse your incontinence is, the worse your depression is expected to be (1) (2).
There are different types of incontinence, the most common are: stress incontinence: leaking small amounts of urine when you laugh, cough, sneeze or exercise and overactive bladder: when you can’t “hold on” or have to pee more often than is normal.
Stress incontinence is more common amongst women who participate in impact exercise – (3). This doesn’t mean you have to give up running, tennis or Zumba, but, it does mean you should ask for help. It is vital that women are physically active to prevent conditions like cardiovascular disease and diabetes. We know that the worse a woman’s leaking is, the less likely she is to exercise. (4).
A normal adult bladder can hold between 300-400ml of urine. It empties typically about 8 times a day and once at night – so if you are peeing more often than that, or if you are up more than once in the night then it’s worth speaking to your GP. (5).
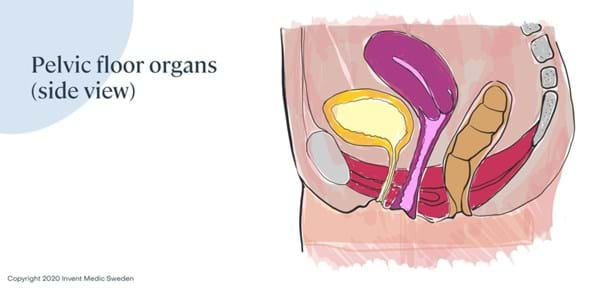
Once your bladder is nearly full, about every 3-4 hours, nerves tell your brain that you need to go to the toilet. Once you sit on the toilet, your pelvic floor muscles relax and the muscle in the bladder wall contracts, squeezing the pee out until the bladder is completely empty. So, if your bladder isn’t properly emptied, if you have to strain to pee, if peeing is painful, if there isn’t much urine or you have to go to the toilet frequently – then you should see your GP.
Some people are sensitive to food and drinks – caffeine, carbonated drinks, artificial sweeteners, and alcohol are all known bladder irritants. (6). Some people try to drink less to reduce their symptoms. However, concentrated urine, the dark yellow or orange pee you see if you are dehydrated, is a bladder irritant. So, not drinking enough can make symptoms worse. (7). Urine should be pale yellow or clear if it is darker then drink more water!
Urinary tract infections, menopause and pregnancy, can all affect bladder function. We do know that pelvic floor exercises can help reduce leaking, urgency and the frequency of peeing, so please, get them done! (8).
We know that embarrassment often prevents people from speaking to their doctor about their incontinence – which is a shame because there are simple things you can do to help. So, please, don’t put up with it. (9).
References
(1) Coyne KS, Sexton CC, Irwin DE, et al. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008;101:1388–95.Sexton CC, Coyne KS, Vats V, et al. Impact of overactive bladder on work productivity in the United States: results from EpiLUTS. Am J Manag Care. 2009;15:S98–107.
(2) 30. Markland AD, Goode PS, Redden DT, et al. Prevalence of urinary incontinence in men: results from the national health and nutrition examination survey. J Urol. 2010;184:1022–7. Melville JL, Delaney K, Newton K, Katon W. Incontinence severity and major depression in incontinent women. Obstet Gynecol. 2005;106:585–92. Melville JL, Fan MY, Rau H, et al. Major depression and urinary incontinence in women: temporal associations in an epidemiologic sample. Am J Obstet Gynecol. 2009;201:490 e1–7. Sung VW, West DS, Hernandez AL, et al. Association between urinary incontinence and depressive symptoms in overweight and obese women. Am J Obstet Gynecol. 2009;200:557 e1–5.
(3) Jacome C, Oliveira D, Marques A, Sa-Couto P. Prevalence and impact of urinary incontinence among female athletes. Int J Gynaecol Obstet. 2011;114:60–3. Nygaard IE, Thompson FL, Svengalis SL, Albright JP. Urinary incontinence in elite nulliparous athletes. Obstet Gynecol. 1994;84:183–7.Carls C. The prevalence of stress urinary incontinence in high school and college-age female athletes in the midwest: implications for education and prevention. Urologic Nursing. 2007;27:21–4. Thyssen HH, Clevin L, Olesen S, Lose G. Urinary incontinence in elite female athletes and dancers. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:15–7.
(4) Nygaard I, Girts T, Fultz NH, et al. Is urinary incontinence a barrier to exercise in women? Obstet Gynecol. 2005;106:307–14.
(5) Fitzgerald MP, Stablein U, Brubaker L. Urinary habits among asymptomatic women. Am J Obstet Gynecol. 2002;187:1384–8.Latini JM, Mueller E, Lux MM, et al. Voiding frequency in a sample of asymptomatic American men. J Urol. 2004;172:980–4. Lukacz ES, Whitcomb EL, Lawrence JM, et al. Urinary frequency in community-dwelling women: what is normal? Am J Obstet Gynecol. 2009;200:552 e1–7.
(6) Lee JG, Wein AJ, Levin RM. The effect of caffeine on the contractile response of the rabbit urinary bladder to field stimulation. Gen Pharmacol. 1993;24:1007–11.Arya LA, Myers DL, Jackson ND. Dietary caffeine intake and the risk for detrusor instability: a case-control study. Obstet Gynecol. 2000;96:85–9. Dallosso HM, McGrother CW, Matthews RJ, Donaldson MM. The association of diet and other lifestyle factors with overactive bladder and stress incontinence: a longitudinal study in women. BJU Int. 2003;92:69–77. Dasgupta J, Elliott RA, Doshani A, Tincello DG. Enhancement of rat bladder contraction by artificial sweeteners via increased extracellular Ca2+ influx. Toxicol Appl Pharmacol. 2006;217:216–24. Lohsiriwat S, Hirunsai M, Chaiyaprasithi B. Effect of caffeine on bladder function in patients with overactive bladder symptoms. Urol Ann. 2011;3:14–8. Shorter B, Lesser M, Moldwin RM, Kushner L. Effect of comestibles on symptoms of interstitial cystitis. J Urol. 2007;178:145–52.
(7) Beetz R. Mild dehydration: a risk factor of urinary tract infection? Eur J Clin Nutr. 2003;57(Suppl 2):S52–8
(8) Wyman JF, Burgio KL, Newman DK. Practical aspects of lifestyle modifications and behavioural interventions in the treatment of overactive bladder and urgency urinary incontinence. Int J Clin Pract. 2009;63:1177–91 Jackson SL, Scholes D, Boyko EJ, et al. Predictors of urinary incontinence in a prospective cohort of postmenopausal women. Obstet Gynecol. 2006;108:855–62. Moore EE, Hawes SE, Scholes D, et al. Sexual intercourse and risk of symptomatic urinary tract infection in post-menopausal women. J Gen Intern Med. 2008;23:595–9 Persson J, Wolner-Hanssen P, Rydhstroem H. Obstetric risk factors for stress urinary incontinence: a population-based study. Obstet Gynecol. 2000;96:440–5. [PubMed] [Google Scholar]Meyer S, Schreyer A, De Grandi P, Hohlfeld P. The effects of birth on urinary continence mechanisms and other pelvic-floor characteristics. Obstet Gynecol. 1998;92:613–8. Hannah ME, Hannah WJ, Hodnett ED, et al. Outcomes at 3 months after planned cesarean vs planned vaginal delivery for breech presentation at term: the international randomized Term Breech Trial. JAMA. 2002;287:1822–31. Hirsch AG, Minassian VA, Dilley A, et al. Parity is not associated with urgency with or without urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21:1095–102
(9) Coyne KS, Zhou Z, Thompson C, Versi E. The impact on health-related quality of life of stress, urge and mixed urinary incontinence. BJU Int. 2003;92:731–5 Elstad EA, Taubenberger SP, Botelho EM, Tennstedt SL. Beyond incontinence: the stigma of other urinary symptoms. J Adv Nurs. 2010;66:2460–70. Liberman JN, Hunt TL, Stewart WF, et al. Health-related quality of life among adults with symptoms of overactive bladder: results from a US community-based survey. Urology. 2001;57:1044–50. Wilson MM. Urinary incontinence: a treatise on gender, sexuality, and culture. Clin Geriatr Med. 2004;20:565–70. ix. NICE Quality standard [QS77]. Urinary incontinence in women. January 2015. [Cited 28 August 2018] Available from: https://www.nice.org.uk/guidance/qs77/chapter/Quality-statement-5-Bladder-trainingNewman DK, Borello-France D, Sung VW. Structured behavioral treatment research protocol for women with mixed urinary incontinence and overactive bladder symptoms. Neurourology and Urodynamics. 2017;37:1;14-26. [Cited 28 August 2018] Available from: https://doi.org/10.1002/nau.23244